Blueprint for the AI-enabled EHR
TL;DR
To stay competitive, EHRs must evolve from passive record systems into AI-driven platforms that reduce clinician burnout, improve decisions, and unlock revenue.
This piece covers:
- How AI shifts EHRs from static storage to active clinical and operational copilots
- The seven core EHR building blocks, and how each becomes a launchpad for AI differentiation
- Where to start for fast ROI, with ambient documentation and revenue cycle automation
- How to build a future-proof AI strategy through clear product vision and the right infrastructure partner
Introduction
Electronic Health Records (EHRs) sit at the very heart of a modern healthcare system. They are the system of record that underpins nearly every patient interaction, capturing demographics, documenting encounters, tracking results, and connecting care teams. For decades, EHRs have promised a single source of truth for clinicians, administrators, and patients alike. Yet in practice, many providers experience them as digital filing cabinets: necessary, but often cumbersome and time-consuming.
A new wave of innovation is changing that reality. AI is redefining what an EHR can be, transforming it from a passive repository into an active clinical and administrative copilot. Instead of merely storing information, AI-enabled EHRs can surface insights at the point of care, automate routine tasks, personalize patient engagement, and support clinicians in making better, faster decisions.
This blueprint lays out how organizations can begin that journey. By mapping core functions to the workflows of clinicians, patients, and administrators and layering in AI capabilities it outlines a practical path to move from static record-keeping to real-time intelligence. The goal is straightforward but high-impact: to equip EHR vendors with a future-proof AI strategy that strengthens competitiveness and delights users.
Market landscape: where EHRs stand today
The EHR market in the U.S. is still dominated by a few major players: Epic, Oracle Cerner, and Meditech. Each of these players, along with the smaller challengers, are announcing AI strategies and competing to stay at the forefront of the AI adoption wave coming in healthcare.
- Epic recently unveiled a slate of AI-powered features including an ambient scribe, AI-assisted charting, and revenue cycle management tools, in partnership with Microsoft’s ambient clinical AI.
- Oracle announced its own next-generation AI-driven EHR platform, integrating intelligent automation across patient care and administrative workflows.
- Meditech recently partnered with Commure to embed an AI powered ambient scribe into their mobile EHR application.
- Athenahealth is positioning themselves as "AI-native" with their athenaOne platform for ambulatory providers, designed to enhance clinical summaries, interoperability, and patient engagement.
It can seem like every other week there is a new announcement about AI roadmap developments in healthcare. If you’re an EHR without a meaningful AI strategy, you run the risk of falling behind your competition. But if you are are actively thinking about what a robust AI strategy looks like, you are in luck. Nimble, AI-native EHRs can build and ship features fast and win the hearts and minds of clinicians who are craving ways to make their lives easier and enhance the patient experience. The surge of announcements shows that progress is being made, but also reveals how far the industry still has to go.
Even with all these development efforts underway, a gap still persists.
Despite steady innovation, EHRs remain one of the top drivers of clinician frustration. Providers report burnout from excessive documentation, fragmented workflows, and poor usability. Data fragmentation across systems complicates care coordination, while billing complexity and prior authorization remain major administrative burdens.
In their current form, EHRs excel at storing and retrieving patient data, but fall short when it comes to actively reducing workload or improving decisions. This is the opening for AI. By layering in AI capabilities like intelligent chart review, ambient documentation, predictive analytics, revenue cycle automation, and clinical decision support, EHRs can elevate from static record-keeping to dynamic care platforms.
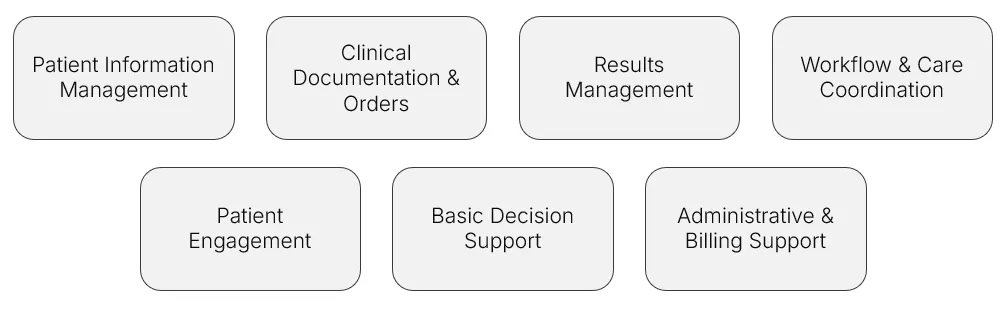
The basic building blocks of an EHR
Every EHR, regardless of vendor or setting, must deliver on a set of foundational capabilities. These represent the minimum viable functions that enable providers to document, coordinate, and bill for care. Without them, an EHR cannot serve as the central nervous system of a health system or practice.
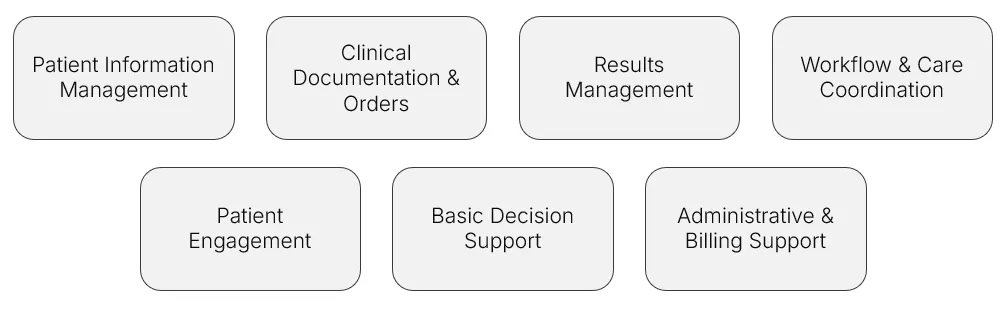
For decades, these functions have been the backbone of electronic records. But today, they represent only the starting point. By supercharging these core capabilities with AI, EHR vendors can stay competitive in the wave of AI adoption and deliver real differentiation.
AI-supercharged building blocks of an EHR
Going forward, every EHR, regardless of vendor or setting, must deliver on a set of AI capabilities. We see each of the basic building blocks of an EHR as an opportunity and entry point to ship differentiated, high-value AI features. Treating these building blocks as launchpads for AI allows you to move fast without starting from scratch. Instead of reinventing the entire product, you can layer intelligence into what already exists, solving problems that matter most to your users, staying competitive in a crowded market, and proving value quickly.
We see each of the basic building blocks of an EHR as an opportunity and entry point to ship differentiated, high-value AI features.
1. Patient information management: from silos to summaries
The problem you're solving: clinicians click through an average of 37 tabs to piece together a patient's story. They spend the first ten minutes of every encounter playing detective, hunting for the last visit note, scrolling through medication lists, and trying to spot what's changed since the last visit.

Your AI solution stack: deploy an intelligent data ingestion agent that automatically pulls and reconciles data from multiple sources. Add a longitudinal patient profile builder that creates a single, chronological narrative of the patient's journey. Top it off with a pre-visit chart reviewer that surfaces exactly what matters for this encounter, before the visit even happens.
What success looks like: Instead of clicking through 37 tabs to reconstruct a patient’s history, Dr. Singh opens a pre-visit profile that highlights the most relevant updates since the last encounter. Medications, problems, labs, and referrals are all synthesized into a clean summary, with AI flagging what’s changed or needs attention. The visit starts with clarity — not detective work.
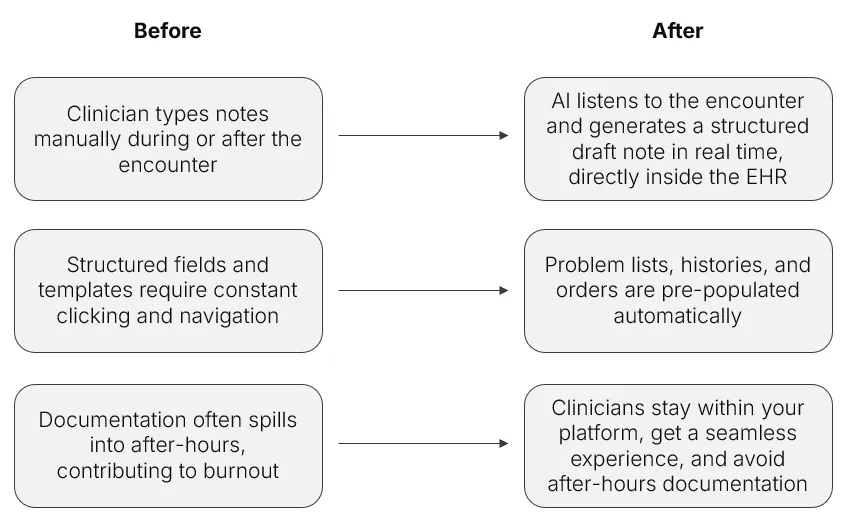
2. Clinical documentation: from typing to talking
The problem you're solving: documentation consumes 35% of a clinician's day. The average emergency physician generates 4,000 mouse clicks per shift. Family physicians finish notes at home 1.5 hours after clinic ends. This isn't sustainable.
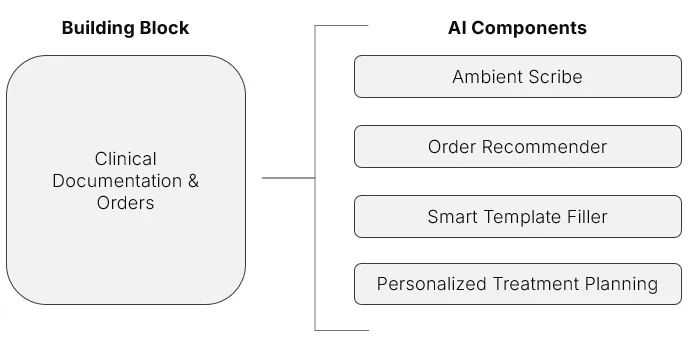
Your AI solution stack: an ambient scribe that captures natural conversation and generates structured notes in real time. Smart template fillers that adapt to specialty and context. An order recommender that suggests next steps based on guidelines and patient history. A personalized treatment planning agent that drafts care plans tailored to each patient's circumstances.
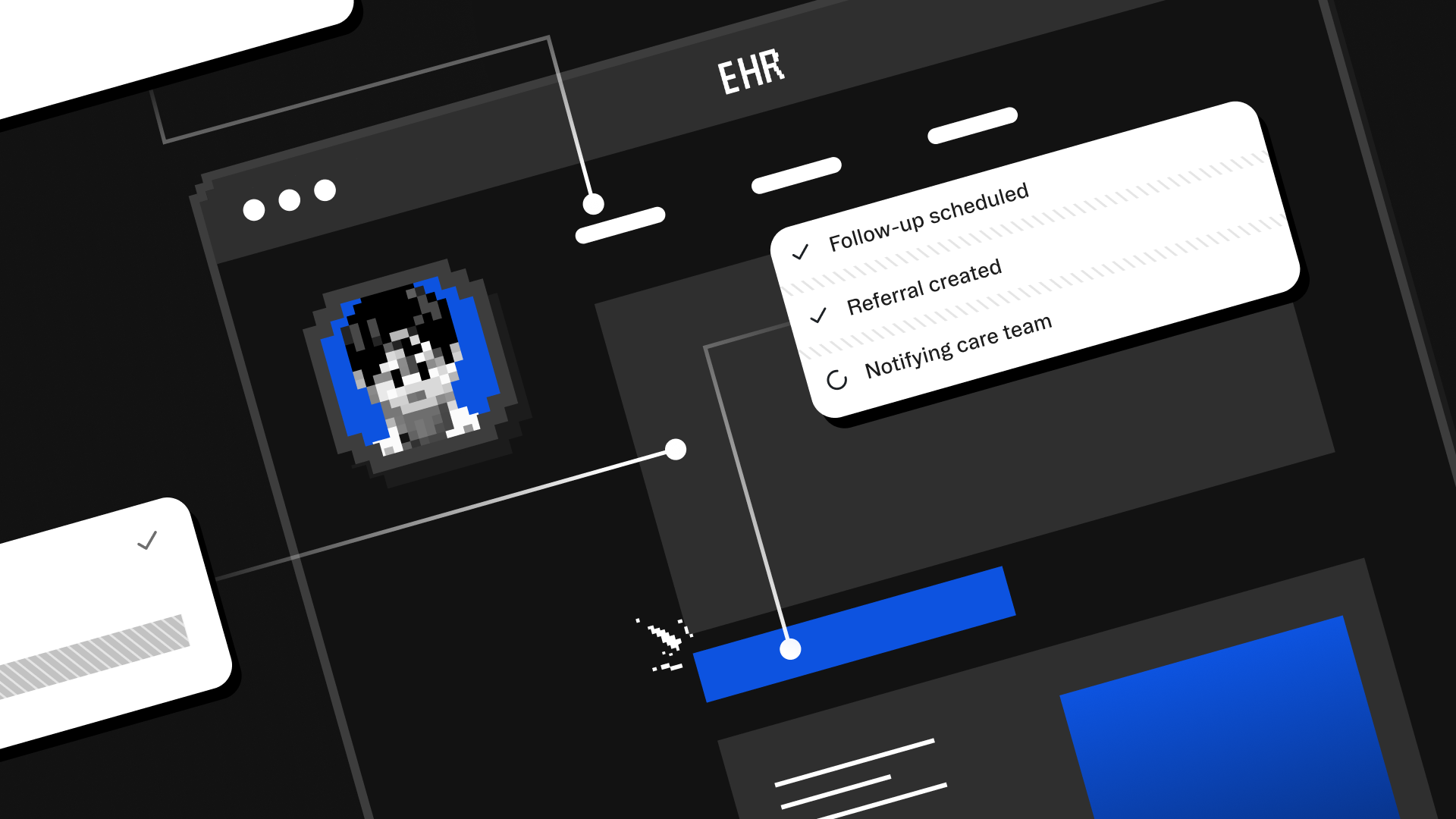
What success looks like: During the visit, Dr. Reyes talks naturally with her patient. Behind the scenes, an ambient scribe captures the encounter, suggests ICD-10 codes, and fills in the note in real time. By the time the patient leaves, the draft is 90% complete, including next steps and orders.
3. Results management: from scanning to synthesizing
The problem you're solving: a hospitalist reviews 150+ lab results daily. An oncologist tracks dozens of tumor markers across multiple patients. Critical trends hide in numerical noise. Abnormal results get buried in the queue.
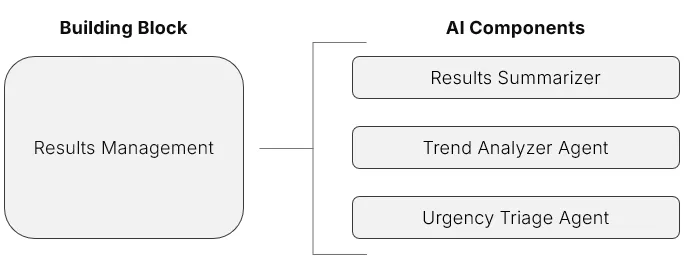
Your AI solution stack: a results summarizer that converts data dumps into clinical narratives. A trend analyzer agent that spots patterns humans miss. An urgency triage system that ensures critical findings never wait.
What success looks like: instead of scanning 47 individual lab values, Dr. Kim sees: "Kidney function declining 15% over 3 weeks, likely medication-related. Consider dose adjustment for metformin. New mild anaemia developing—iron studies recommended." The AI has already identified the pattern, suggested the cause, and recommended next steps.
4. Workflow coordination: from managing to orchestrating
The problem you're solving: care coordination is death by a thousand tasks. Following up on referrals, scheduling tests, writing letters, tracking recommendations—each one stealing minutes that compound into hours.
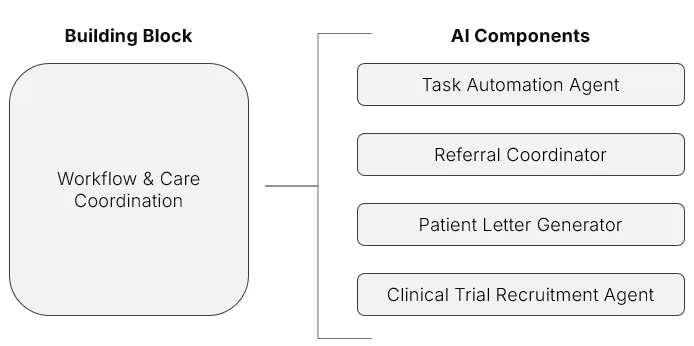
Your AI solution stack: a task automation agent that handles routine follow-ups. A referral coordinator that generates letters and tracks responses. A patient letter generator that writes in plain English. A clinical trial recruitment agent that identifies eligible patients automatically.
What success looks like: when Dr. Johnson orders a cardiology referral, the AI drafts the referral letter with relevant history, schedules the appointment based on urgency, sends the patient instructions in their preferred language, sets follow-up reminders, and alerts Dr. Johnson if the appointment isn't kept. Zero additional clicks required.
5. Patient engagement: from one-size-fits-all to personalized journeys
The problem you're solving: patient portals have just 15%-30% sustained engagement rates. Patients struggle with medical jargon, generic education materials don't resonate, and adherence to care plans remains stubbornly low.

Your AI solution stack: a conversational patient agent for natural language interactions. A personalized education generator that adapts to health literacy levels. An adherence coach that provides timely, contextual nudges.
What success looks like: Maria, recently diagnosed with diabetes, receives education materials written at her reading level, in Spanish, with culturally appropriate meal suggestions. Her AI coach texts her gentle reminders about blood sugar checks, celebrates her victories, and alerts her care team if patterns suggest she's struggling—all before her next appointment.
6. Clinical decision support: from alerts to insights
The problem you're solving: current decision support is crying wolf at scale. Physicians dismiss up to 96% of alerts. Alert fatigue is real, dangerous, and getting worse. Meanwhile, genuine insights that could prevent adverse events get lost in the noise.

Your AI solution stack: a guideline-checking agent that knows context matters. Risk prediction models that forecast, not just flag. A polypharmacy safety checker that understands drug interactions dynamically. A clinical chat assistant that lets clinicians ask questions in plain English.
What success looks like: instead of 47 pop-ups about drug interactions, Dr. Martinez sees one meaningful alert: "This patient's kidney function has declined 20% since starting this medication combination. Three similar patients in your panel developed complications. Consider alternative regimen." The AI learned from outcomes, not just rules.
7. Revenue cycle management: from denials to dollars
The problem you're solving: healthcare organisations lose 5% of revenue to coding errors. Prior authorisation takes 16 hours weekly per physician. First-pass denial rates hit 20%. Every claim rejected is money left on the table and administrative burden added.
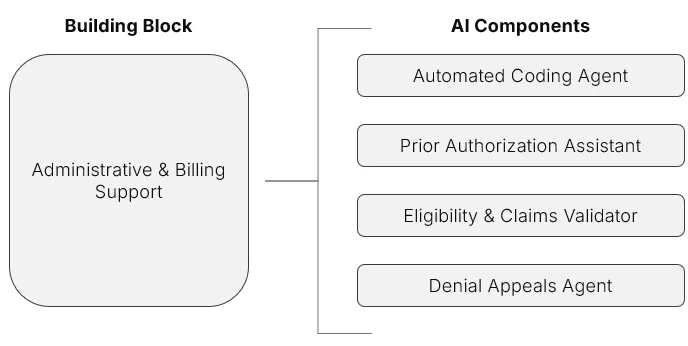
Your AI solution stack: an automated coding agent that extracts codes from documentation in real time. A prior authorisation assistant that generates packets instantly. An eligibility and claims validator that pre-checks before submission. A denial appeals agent that crafts compelling arguments with supporting documentation.
What success looks like: as Dr. Williams completes her note, the AI has already identified the correct ICD-10 and CPT codes, checked them against payer rules, flagged potential prior authorization requirements, and prepared the authorization packet with supporting clinical documentation. Coding accuracy jumps to 98%, prior authorization approval rates hit 91%, and days in AR drop by 30%.
When these supercharged building blocks come together, your EHR becomes more than an archive of information. It functions as an intelligent platform that supports every stakeholder — clinicians, patients, and administrators.
Takeaway: These seven building blocks are no longer just “the basics.” They are the raw material for differentiation. Supercharged with AI, they shift from back-office utilities into intelligent capabilities that delight users and strengthen your competitive edge.
Where to get started?
Of all the AI capabilities to build, we suggest starting with two high-impact use cases: Ambient Scribe and Revenue Cycle Management. These “supercharged” capabilities target two of the biggest pain points for your EHR users — clinician burnout and thin operating margins.
Quick win #1: Ambient Documentation
Every EHR needs an integrated ambient scribe by 2026.
Why this first: every EHR needs an integrated ambient scribe by 2026. There are 120+ point solutions fragmenting the market, but clinicians want it built into their workflow. You have the advantage — you already own the platform.
Integrating an ambient scribe is a quick win for your customers. It reduces the burden of documentation while capturing the rich clinical dialogue that fuels downstream AI augmentation and automation—becoming a critical input for the rest of your AI roadmap.
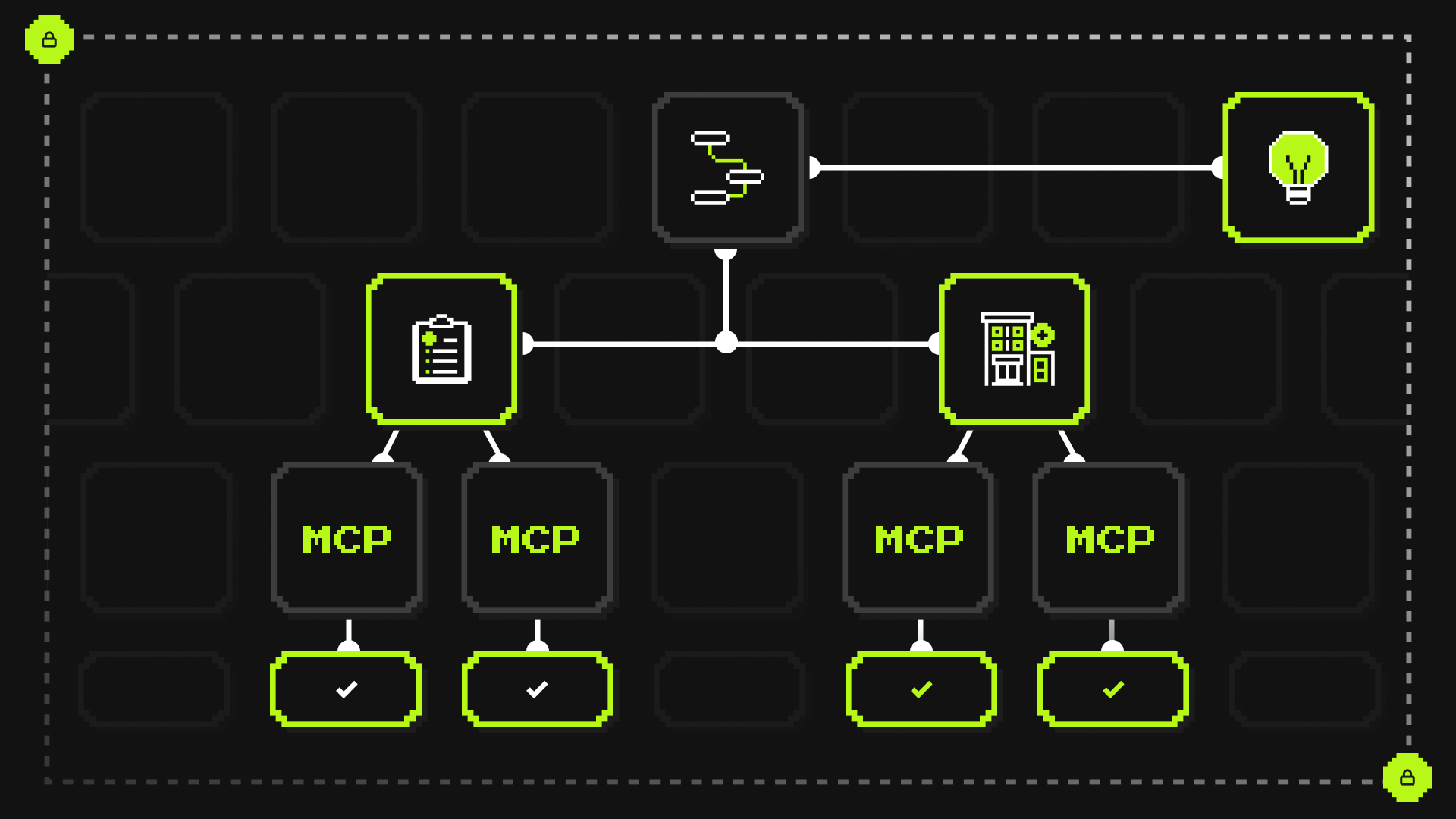
At Corti, we have worked with thousands of developers shipping ambient scribes. We typically see one of two routes to integrate the core functionality into your platform, depending on how much control and speed you need.
Option A: build on APIs for maximum control
Perfect when you want to own every detail of the experience. You control the UI, customize templates by specialty, manage privacy settings, and maintain complete architectural flexibility.
- What you control: UI and UX, prompts and templates, fact extraction, diarization and speaker labels, privacy controls, data retention, languages, redaction.
- Core building blocks: real-time audio streaming, transcript and events, structured fact extraction, note generation, export to your EHR objects.
Quickstart: Build on our API
Option B: embed pre-built for maximum speed
Drop a battle-tested scribe into your encounter screen and ship quickly.
- What you get: a ready UI, real-time transcript, structured note draft, clinician review and accept.
- Good fit when: you want weeks not months, you have a small team, you prefer a proven UX, you are running a pilot with a firm deadline.
Quickstart: Embed Corti Assistant
Quick win #2: revenue cycle automation
Every EHR needs RCM that turns documentation into revenue.
Why this is next: Money talks. While clinician burnout is emotional, revenue is mathematical. Health systems operating on 2% margins will move mountains for a 5% improvement in collections.
If clinician burnout is a top pain point, revenue leakage is right up there with it. Margins across health systems are razor thin, and billing complexity only makes it worse. Most EHRs today support only basic coding capabilities: manual code lookup, rules-based prompts, and claim scrubbing. Coders still spend hours reconciling documentation, fixing errors, and reworking denied claims.
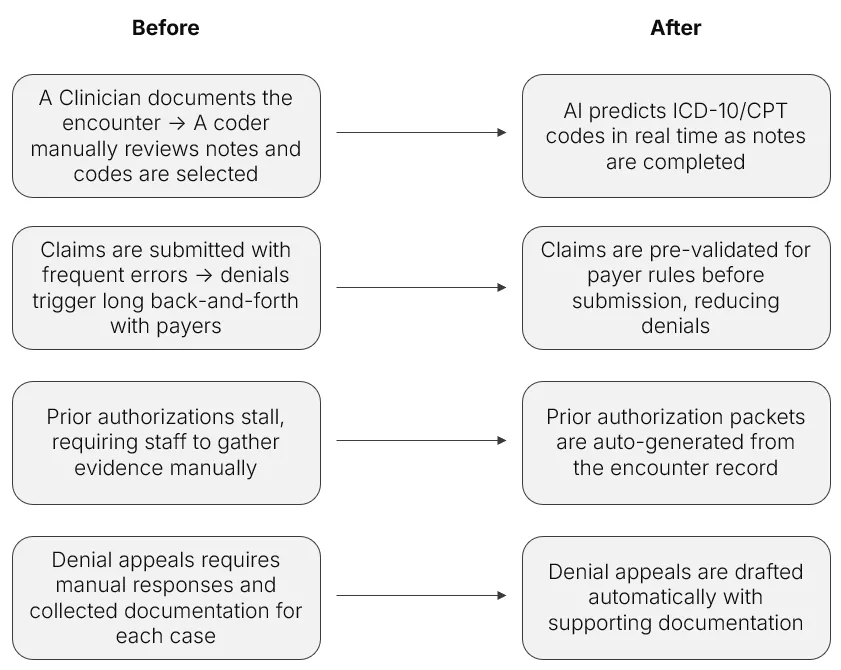
The opportunity for AI is to move from basic code lookups to automated code prediction and claim readiness, reducing errors, speeding billing, and unlocking revenue with much less human effort. An AI-enabled revenue cycle module can transform the financial performance of your provider’s organization by accelerating cash flow and reducing costly rework.
The implementation path:
Start with automated coding. it's the lowest-hanging fruit with immediate ROI. As documentation completes, AI extracts codes in real time, reducing coding backlogs from days to minutes.
Layer in prior authorization next. The documentation for prior authorization already exists in your EHR; AI just needs to package it correctly. What takes staff hours becomes an automated process.
Add claims validation. Check every claim against payer rules before submission. Catch errors before they become denials.
Lastly, add in denial management. Once a denial hits, AI can draft appeals automatically using the structured data already in the EHR. What once required hours of manual review and documentation now takes minutes, freeing up staff while accelerating reimbursement.
How to get started building?
For EHR vendors, the challenge is not whether to build AI but how to begin. End user demand for AI in their EHR is already here. Clinicians and health systems expect smarter documentation, more efficient workflows, and intelligent insights at the point of care.
Two areas matter most when you're getting started: a clear product vision and the right technology partner.
Clear product strategy
AI must be more than a bolt-on feature. It should sit at the center of your product strategy. Start by answering a few core questions:
- What role will AI play in differentiating your EHR in the market?
- Which problems for clinicians or administrators are you solving first?
- How will AI features align with your customers’ goals, whether reducing burnout, supporting value-based care, or accelerating revenue cycle management?
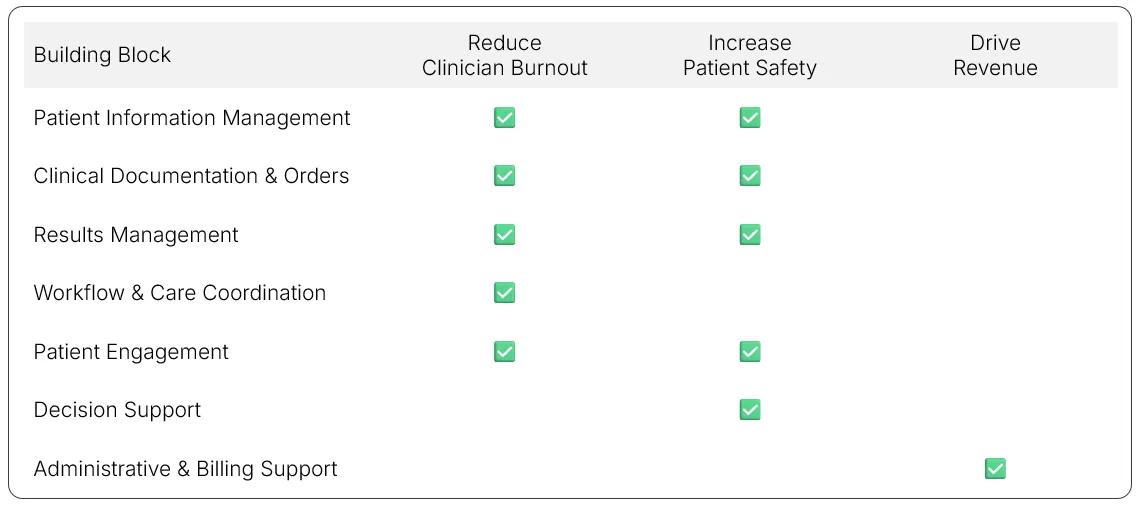
A future-proof AI strategy delivers on three core promises to your end users: reduce clinician burnout, increase patient safety, and drive revenue. Each of these outcomes maps directly to the needs of the people who rely on your platform every day. For clinicians, AI removes clicks. For patients, it personalizes engagement. For administrators, it automates the revenue cycle.
The table below shows how the AI-enabled versions of the seven core building blocks deliver value across these three outcomes that matter most to your users — clinicians, administrators, and patients.
Selecting AI Infrastructure
Most EHR vendors will not build their own large language models. Instead, they will partner and integrate capabilities via APIs. Choosing the right partner is one of the most important early decisions you will make. Consider:
- Which AI platform or LLM provider best matches your requirements for scalability, latency, and reliability?
- Does the provider have the compliance posture you need, including HIPAA, GDPR, SOC2, and regional data residency?
- How will you access their models — through APIs, SDKs, or managed services — and can those integrations scale with your customer base?
- Does the provider offer roadmap alignment, healthcare-specific fine-tuning, and transparent performance metrics?
- How will you monitor and govern models in production as the provider pushes updates?
Getting these decisions right ensures you are not just embedding AI, but embedding it in a way that is scalable, compliant, and sustainable.
Conclusion: The path forward
There is an AI wave moving through healthcare, and it is moving fast. Every major player is shipping AI features, from ambient scribing to revenue cycle automation. Customers now expect their EHRs to do more than store data. They expect intelligence at every step of the care journey.
If you cannot keep up, you risk losing ground. Health systems will choose platforms that make clinicians’ lives easier, deliver measurable ROI, and improve the patient experience. To stay competitive, EHR vendors must move quickly, but not recklessly. Working with a partner that understands the complexity of healthcare and refuses to cut corners on safety, compliance, and privacy is non-negotiable.
This market will not reward hesitation. Without a clear AI strategy, you will not just fall behind, you will risk irrelevance. The vendors who lead will be those who build AI into the core of their platforms, not as a pilot or experiment, but as the foundation of the next generation of EHRs.
The AI era in healthcare is already here. Decide how you will ride the wave — with a blueprint, a trusted partner, and a strategy that can scale.
Take action today
- For quick validation: start prototyping in our AI studio
- For strategic planning: book a scoping call with our healthcare AI experts
- For technical teams: dive into our documentation and start building